This story pairs with “Similar but different: The opioid epidemic across America“

Jon Redd grew up the oldest of six kids in the suburbs of Salt Lake City. His father was a corporate attorney and they lived in a nice house. “We had everything going for us in the world,” he said.
Now, four of the six children in his family are suffering from addiction.
Redd received a bachelor’s degree in psychology from the University of Utah and earned certifications to become a licensed substance abuse counselor. After deciding he wanted to do something else, Redd received a master’s degree from Brigham Young University and went into medical sales.
Redd said working with doctors gave him easy access to drugs like oxycodone. Initially, it was just prescription pills, but Redd began drinking too.
In 2013, Redd was diagnosed with stage 4 thyroid cancer. Surgery and complications after surgery led to opioid prescriptions. “I quickly started using opioids, not only for pain but as a way of coping with the emotional distress of having cancer and the fear that accompanied it,” Redd said.
But after successfully beating cancer, Redd was still struggling with another disease: his addiction.
During 2018, 128 people died per day in the United States from opioid overdose, according to the National Institute on Drug Abuse. Hundreds of thousands of people struggle with opioid addiction. It’s an addiction that doesn’t affect one gender, race, demographic or class.
Opioids are narcotic substances that are typically prescribed to treat pain. Common types are oxycodone, morphine, fentanyl and codeine commonly found in pills like OxyContin, Percocet and Lortab.
Malyce Warner said how we deal with pain plays a large factor in opioid use and misuse. “Across the nation, we view pain as a very negative thing. And so we don’t want to feel pain. If we feel pain, something’s wrong.”
A former prevention specialist at the Utah County Department of Drug and Alcohol Prevention and Treatment, Warner specialized in opioid overdose prevention and community coalition work.
Warner said feeling pain should be expected, especially after a major surgery. People rate hospitals based on their pain and doctors try to control people’s pain. When ratings lower, doctors will try to raise those ratings. To do so, they prescribe larger amounts of opioids to further decrease patients’ pain. For some individuals, this increase in opioid prescriptions eventually leads to dependence and addiction.
As the opioid epidemic spread across the nation, Utah reacted quickly, treating the epidemic as a public health crisis. In 2017, Utah Attorney General Sean Reyes organized the Utah Opioid Task Force to combat the epidemic through proposed legislation, innovation, prosecution and law enforcement.
In 2017, the Utah Senate passed SB258, which requires the Department of Health to establish guidelines for prescribing opioids and opioid antagonists, which block the effects of opioids.
The Senate also passed Utah Code sections that urged health insurers to develop and enact policies that minimize opioid addiction and overdose risk. These policies include non-narcotic treatment alternatives for patients with chronic pain and medication-assisted treatment for opioid dependence disorders.
Other bills and code sections have been passed that regulate who is authorized to write prescriptions, education for controlled substance prescribers, overdose reporting, Medicaid policies, treatment programs and emergency treatment.
Utah County Commissioner Nathan Ivie said it is important to utilize current resources to better dispose of drugs, reduce prescription rates in hospitals and increase pre-screening so people better understand the disease of addiction.
Ivie said doctors and pharmacists need to play a larger role in fighting the epidemic, something Utah County is aiming to do by educating doctors and pharmacists.
These conversations are often difficult, Warner said. “It’s hard to have a community member come in and tell a physician they are prescribing wrong. It has to come from a professional that is on their same level.”
To do so, Warner said medical schools are increasing opioid education like how to prescribe opioids and the effects of opioids on patients. Despite these measures, Warner said there are still many things that could work to help address the epidemic. One measure is syringe exchange programs, which have yet to be established, an issue she credits to Utah’s dominant conservative opinion.
“I know we get a lot of grief sometimes for some of our regulations and rules and policies that we have as a state. But we also have some of the lowest use rates regarding substances,” Warner said.
Educating the community is just as important as educating doctors and pharmacists, according to Warner.
To do so, the Utah Department of Health created a campaign called Stop the Opidemic in 2016. The campaign involved putting up fact-spreading billboards across the state as well as sharing statistics, stories, risks, treatment and information regarding opioids and opioid addiction on its website.
“There was an ‘all is well in Zion’ mentality,” Ivie said. “Through (these campaigns) we have been able to turn that around. The family mentality has helped that occur because we rally around people.”
Legislation and government-funded campaigns work to prevent the spread of opioid misuse and overdose, but what is done for those who are already suffering from this disease?
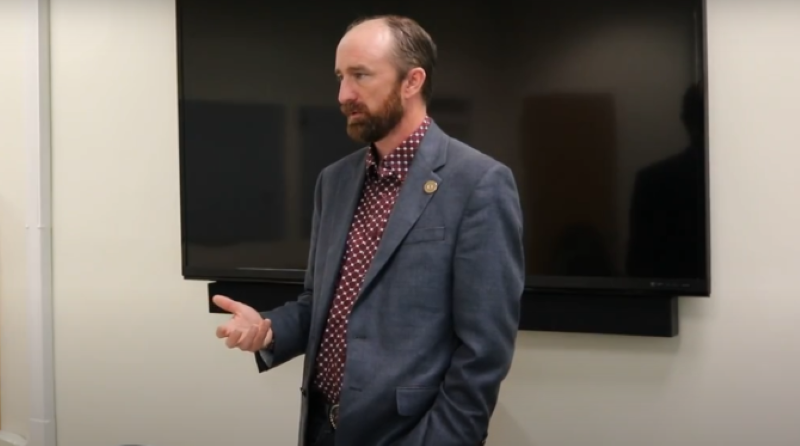
Redd entered Renaissance Ranch at age 43. His wife had just gone through an outpatient program. He had lost multiple jobs and was close to losing his family. “I’d lost a lot of things that were important to me,” he said.
He began with a 60-day inpatient program. The ranch is spiritually centered, Redd said. “We really focus on a higher power and God. And we don’t shy away from that.”
Patients also go through cognitive behavioral, emotional and family therapy while going through the 12 steps of Alcoholics Anonymous (AA).
“We look at it like not only do they have a mental and physical malady but also a spiritual malady. We try to connect their spirit. We try to get their minds right and their bodies,” Redd said.
Regardless of religious affiliation, the Ranch encourages connecting to a higher power, whatever it may be. Patients are taken each week to whatever religious service they would like to attend.
While building that connection, Renaissance Ranch works to undo the shame many patients feel when they enter the facility.
“The biggest problem that we need to face is shame, which means that people may have this disease but not be comfortable to talk about it. They don’t look at it as a disease. They look at it as a moral weakness,” Redd said.
Redd believes shame is something rampant in Utah’s culture. He said his shame led to his unwillingness to talk with people about what he describes as his “disease.”
“We don’t talk about things. We don’t talk about the struggles, the problems. We kind of sweep them under the rug, and we put on a good face for the community,” he said.
Warner said she believes Utah faces many unique difficulties, like shame culture, regarding the opioid epidemic. She partially credits Utah’s culture and the dominant religious affiliation to these difficulties. According to the Pew Research Center, 55% of adults in Utah identify as members of The Church of Jesus Christ of Latter-day Saints.
Warner said because of the prominence of the Latter-day Saint faith, “oftentimes drug use is seen as a morality issue; bad people doing bad things.”
This view of drug use can get in the way of how people in the community feel and react, she said.
The Church offers its own Addiction Recovery Program that focuses on 12 steps based in “gospel principles,” according to the Church’s website. These steps closely align with the 12 steps of Alcoholics Anonymous.
The Church’s program is open to anyone regardless of Church activity or membership. Senior missionary couples run weekly 12-step recovery support meetings for both those struggling with the disease and their family members.
These missionary couples run, organize and plan recovery meetings based on principles found in the Church’s workbook, which is written by those in recovery, according to Thomas and Carole Colemere who serve as coordinators for the Salt Lake Addiction Recovery Mission.
The Colemeres said they are not experts in counseling or addiction recovery but focus on the emotional side of addiction; building connections and love between those in recovery, their families and the community.

There are numerous rehabilitation centers in operation throughout Utah that all offer different forms and principles of treatment. Jerry Costly is the director of De Novo, an addiction treatment center in Salt Lake City.
“I believe we should be willing to meet someone as best we can as long as it doesn’t endanger the person more than they would already be in danger. We should meet them where they’re at,” Costly said.
Costly tries to do what he called anthropological studies of patients that come to De Novo. “We need to know how this person sees the world, how they view the world and how they view their addiction.”
Treatment should be strength-based, Costly said, focusing on the strengths a person has and building on those, rather than on weakness and what needs to change.
To do this, Costly often focuses on the drug doing the most damage to a patient, if there are multiple drugs. Costly said it’s important in treatment to determine why a person has turned to drugs.
“Drugs can do a wonderful job helping you meet new people, helping you drop your inhibitions, relieve boredom for people who decide to sell them; they’re a great way to make quick money. There are all kinds of legitimate needs that drugs can meet,” he said.
Costly said once the need for drugs is determined, he can help patients figure out how to meet those needs without drugs. He said opioid addiction is a universal problem that “cuts across all cultures, all genders, all expressions of gender and all socioeconomic statuses.” Treatment needs to be more available, he said.
Warner also recognized that, despite the efforts Utah has made to address this epidemic, there is still more that could be done, especially by the community. “It’s important to know what is going on in your community,” she said.
Public health often gets so caught up in saving people, Warner said, that the people who are struggling are not heard. “You have (to) have them at the table.”
The opposite of addiction is connection, Redd said. Addiction needs to be discussed openly. “Once we start talking about it, we can address it and get help.”
Moving forward, Warner said there are some negative consequences to the positive efforts being implemented. People who suffer from chronic pain are facing difficulties receiving their pain medication because of harsh restrictions at pharmacies. “Some would argue we’ve gone too far or too extreme so that now we’re harming those who genuinely need opioids.”
Warner said this is something that will need to be addressed in the future. “Opioids have their place and people who need them need to be able to access them.”
Read more from this series:




