Editor’s note: This story pairs with another titled “Chaffetz: Obamacare was sold on a lie.”
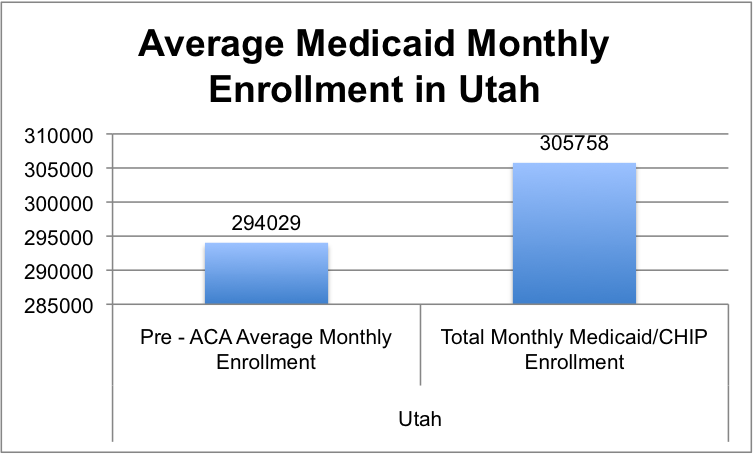
Medicare and Medicaid recipients are wondering what will happen when Congress repeals Obamacare, particularly since discussion about its Republican-engineered replacement includes the possibility that millions will lose their coverage.
President Barack Obama’s Patient Protection and Affordable Care Act, dubbed ObamaCare, was signed into law on March 23, 2010. The healthcare reform plan promised healthcare expansion coverage to all Americans, including those who could not afford their own.
Those less able to afford insurance on their own applied for subsidies to help them cover the cost of their premiums. The subsidized healthcare coverage of the Affordable Care Act shifted the weight of those premiums to help cover the cost of the coverage.
But the money had to come from somewhere, and that somewhere came out of the pockets of the hardworking Americans able to pay for their own insurance, according to some who have seen their health premiums skyrocket.
Mark Mcguire, owner of Intermountain Orthopedic Care in Orem, said rapidly-rising premiums didn’t sit well with his customers, so many boosted their deductibles.
“On my own personal policy, I have a $5,000 deductible, and we’ve seen them even as high as $10,000,” Mcguire said.
When he started his business 18 years ago, a common deductible for an insurance plan was around $250.
Mcguire said unless someone has a really bad accident or needs a major surgery, the cost of covering medical expenses will come out of their own pocket.
“I’m paying $17,000 a year for insurance that I never get to even use,” Mcguire said.
In another cost-cutting move, insurance companies have reduced the amount they reimburse healthcare suppliers for their products. Mcguire, a healthcare supplier himself, said his business has suffered greatly since Obamacare came into effect.
Medicaid was designed to provide health insurance coverage to low-income and elderly Americans. Initially, healthcare providers were promised reimbursement for Medicaid patients. However, because of the reduced reimbursement funds from insurance companies, that’s not the case any longer, and this forced many businesses to turn down Medicaid patients.
Mcguire said for a particular product that costs $500, he might only get reimbursed $300 for that same item. He also said many providers decided the Medicaid reimbursement wasn’t covering their costs, so they stopped providing services for those patients. The same holds true with some private insurance companies.
“People come in and say they need a knee brace and ‘I have XYZ company (as the insurer),'” Mcguire said. “I’m sorry, I cannot help you because I don’t bill that company anymore, because they don’t pay me enough.”
While all insurance companies made things difficult on their customers, Mcguire said Medicaid suffered the most because its federal funding was cut to implement the Affordable Care Act.
It got worse. Insurance companies began taking money back from suppliers and started an auditing program that would take suppliers up to four and a half years to go through an appeal process to get their money back.
Mcguire said a lot of doctors dropped Medicare and Medicaid patients, and that a lot of suppliers don’t even deal with those patients anymore because of the hassle.
While many medical providers have become more selective about accepting certain insurance coverages, Spanish Fork family medicine practitioner Tracy Frandsen chose to see the optimism of the elephant in the room of how the Affordable Care Act has helped his patients.
“There have been some good things,” Frandsen said. “The things that were most desirable to people (with the Affordable Care Act) went into effect first.”
It’s the difficult things, he said, that have only started to come into effect. Frandsen said things like children’s ability to stay on their parents insurance until age 26, preventative care and the elimination of pre-existing conditions as a reason to deny coverage have been helpful for his patients.
While premiums and deductibles took a rise on one end of the spectrum, out-of-pocket expenses for preventative care went down on the other, he said. This was helpful for his patients to be able to receive services like pap smears and mammograms for so little cost.
CNN reported that “doctors have long complained about many rules and regulations that take them away from providing care for their patients.”
Frandsen said the surtaxes that were added to insurance plans have put a weight on his practice. He said there are more than 100 employees in his medical group, and the Affordable Care Act required the company to pay a certain tax based on the number of employees, so all of them could get healthcare coverage.
They almost lose money taking Medicare and Medicaid patients, and they look at it as somewhat of a community service that they provide, Frandsen said. He explained they get paid some, but that it’s not an overly-generous sum.
“We’re unable to do much in terms of paying our employees or our salaries with Medicaid,” Frandsen said.
As Republicans in Congress work on legislation to replace Obamacare, Frandsen said he would hate to see them do away with things like no pre-existing conditions and children’s parental coverage until they’re 26. He said finding a way to insure everyone is a different question on its own.




